CHICAGO – A groundbreaking study published in the Annals of Emergency Medicine reveals a significant disconnect between public awareness and uptake of the shingles vaccine, particularly among individuals seeking care in emergency departments (EDs). The research, led by Michael Gottlieb, MD, at Rush University Medical Center in Chicago, highlights a critical public health opportunity to boost vaccination rates by leveraging the ED setting and addressing the Shingles Vaccination Gap.
The multicenter study surveyed over 1,600 patients aged 50 and older across 10 U.S. emergency departments. It found that while an impressive 87.1% of these patients were aware of the shingles vaccine, only 45.6% had actually received it. This substantial gap underscores a missed opportunity to protect a vulnerable population from the painful and potentially debilitating effects of herpes zoster, commonly known as shingles. Bridging this Shingles Vaccination Gap is essential for effective herpes zoster prevention.
Addressing the Shingles Vaccination Gap in Emergency Departments
The findings from this news report paint a stark picture: despite widespread knowledge about the shingles vaccine, a considerable portion of eligible individuals remain unvaccinated, contributing to the ongoing Shingles Vaccination Gap. Researchers noted that patients with health insurance and those who were older were more likely to be aware of and have received the vaccine. Conversely, individuals who spoke Spanish or other non-English languages had lower awareness. The study also pointed to vaccination disparities, with Black participants showing lower odds of receiving the vaccine compared to other groups.
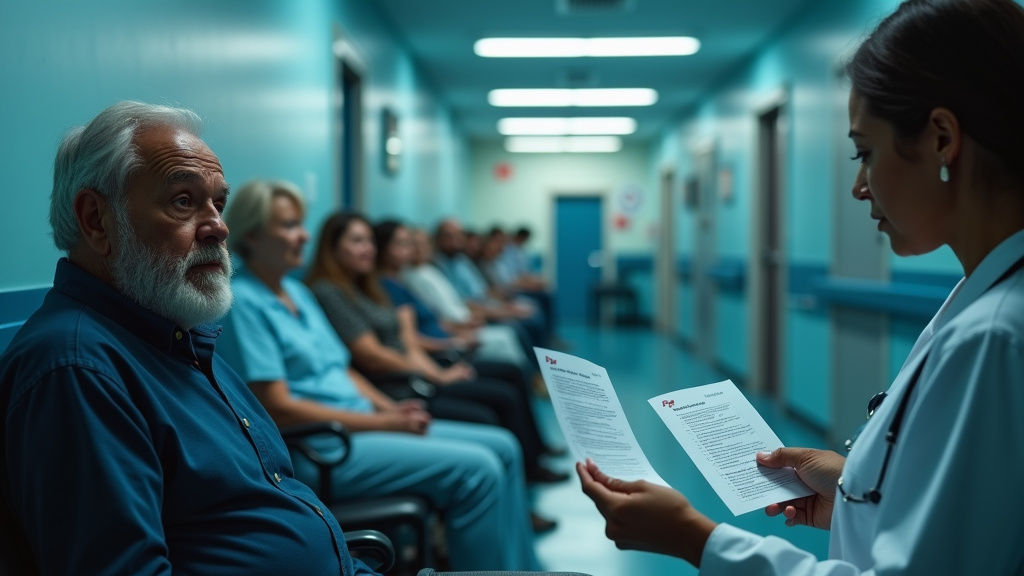
Notably, the research indicated that nearly 40% of unvaccinated patients expressed interest in receiving the shingles vaccine during their current ED visit. This suggests that emergency departments, often seen as a last resort for care, could serve as a vital point for shingles vaccine administration, especially for individuals who may lack consistent access to primary care physicians or face other barriers to vaccination, thus narrowing the Shingles Vaccination Gap.
Why Are Shingles Vaccine Uptake Rates So Low? Barriers and Opportunities
Several factors likely contribute to the low vaccination rates and the prevalent Shingles Vaccination Gap. A systematic review on shingles vaccine uptake identified barriers such as race/ethnicity, socioeconomic disparities, and limited knowledge about the disease and vaccine. In the context of the ED, lack of a regular healthcare provider and limited health insurance also play a significant role, as suggested by previous research indicating higher vaccination rates among those with insurance and consistent primary care access, highlighting a clear public health opportunity.
The expressed willingness of ED patients to receive vaccinations on-site presents a compelling solution to the Shingles Vaccination Gap. By offering the shingles vaccine within emergency departments, healthcare systems could tap into a patient population that is already seeking medical attention, potentially overcoming logistical hurdles like appointment scheduling and transportation. This approach could be particularly effective for underserved communities who rely more heavily on EDs for their healthcare needs, representing a key healthcare intervention point.
The Serious Nature of Shingles and Its Complications
Shingles, caused by the reactivation of the varicella-zoster virus, is far more than just a rash. It can lead to severe complications, including chronic nerve pain known as postherpetic neuralgia (PHN), which can persist for months or years. Other serious consequences can include vision loss, facial paralysis, hearing impairment, brain inflammation (encephalitis), and in rare cases, death. Addressing the Shingles Vaccination Gap is crucial to preventing these severe outcomes.
Recent editorial commentary and research also suggest a link between shingles and increased risks for cardiovascular events, including heart attack and stroke, as well as a potential association with vascular dementia. These potential long-term health impacts underscore the critical importance of vaccination, not only to prevent the acute illness but also to mitigate these more severe outcomes. Historically, ED visits for shingles-related issues have been significant, carrying substantial healthcare costs, further emphasizing the economic and public health rationale for preventative measures to close the Shingles Vaccination Gap.
Recommendations and Future Directions for Closing the Shingles Vaccination Gap
The Centers for Disease Control and Prevention (CDC) recommends the Shingrix vaccine, administered in two doses, for all adults aged 50 and older, and for adults 19 years and older who are immunocompromised. The vaccine is highly effective, offering strong protection against shingles and its complications. Increasing shingles vaccine awareness is vital to reduce the Shingles Vaccination Gap.
The study from Chicago and related analyses highlight that the ED is an underutilized setting for public health interventions like vaccination. Implementing on-site vaccination programs within EDs could address current vaccination gaps, improve access for hard-to-reach populations, and ultimately reduce the incidence of shingles and its associated morbidity, mortality, and healthcare costs, thereby narrowing the Shingles Vaccination Gap.
Conclusion: Overcoming the Shingles Vaccination Gap
The low shingles vaccination rates identified in emergency departments represent a critical public health challenge and a significant Shingles Vaccination Gap. However, the high awareness of the shingles vaccine and the expressed willingness of patients to receive it during ED visits offer a promising pathway forward. By exploring and implementing on-site vaccination strategies in emergency settings, healthcare providers can play a pivotal role in protecting more individuals from the serious consequences of shingles, thereby enhancing overall community health and addressing the persistent Shingles Vaccination Gap.